Den 4/10 skall Södra Älvsborgs sjukhus, SÄS, tillsammans med Försvarsmakten genomföra katastrofövningen LIV 2019. Scenariot och skadeutfallet kommer vara av den omfattningen att sjukhuset måste förbereda sig på att genomföra vård utiifrån andra principer och vårdkvalitet än vad som är aktuellt i vardagen.
En PDF som visar hur vi förberett oss på anestesikliniken inför detta
Företaget Lifeflight som bedriver ambulanshelikoptrar och ambulansflyg i Australien hade hört om kursen och besökte oss i år och berättade om sin HEMS verksamhet. Flera svenska läkare har arbetat åt organisationen tidigare och man har från företagets sida varit så nöjd med detta att man nu erbjuder randning för ST läkare i en mer regelbunden form.
Efter genomförd kurs kan du således ansöka om tjänst som kan tillgodoräknas som randning (självfallet finns möjlighet även för specialister) och om du blir antagen får du hjälp av företaget med de formaliteter i form av ansökningar som behövs för att få arbeta i Australien. Mer information under kursen.
This video appeared on Twitter recently. Ignoring for a moment that it really is just to good to be true (and probably is not).
One good reaction was "I was laughing till I realised Ive seen a lot of anesthesia inductions go about like this". That reflection is so spot on: Many of our most critical procedures go like this. In Swedish I call it "hoppsan-medicin" which translates to something like "Ooops-care". So we see similarities that are not good. But that is just the immediate analysis..
Going back to our pilot and while laughing at him, you have got to hand it to him that he is idetifying and correcting a critical problem quicker than most would, at the same time as he is jibbering on.. (a junior pilot would probably crash the plane 5 out of 10 times with that error)
What does the experienced pilots behaviour tell us? For one thing, he is probably an extremely experienced pilot. Having done this tens of thousands of times before, he uses something bordering on "Gaze-heuristics" (extreme pattern recognition, catching a ball etc). With experience, they work fine, in aviation and CC alike. Problem is first and most obvious, following a checklist will minimize the likelihood of trying to take off with flaps up. But a not so obvious one is a pilot like this is just not mentally really there (obvious in the video) and the Big problem for the passangers is when he experiences a(nother) major problem or anything that overwhelms his interior autopilot and demands his mental/cortical awareness. Deviating to a more structured cortical approach, our pilot very much starts in the "mental backseat"..
How does this relates to our #Scandinaviananaesthetist, the one who has done 15000 ETIs & thousands of emergency RSIs etc etc... .
Our experienced colleague, doing just another roadside or ED TBI RSI.. Sometimes you see the same thing with him/her and sometimes you can identify a big risk that he is just not mentally there. (Sorry to disillusion those of you who still find it exciting, after 15000 you just dont get that all worked up any more..) And things go fine, even when not entirely according to plan, "Gaze-heuristics" and internal autopliots in good effect. Up until it is not fine, wich allmost never happens.. Wich makes us believe (us back in the plane or in the ED bed), that everything is just fine.. Marginal safety improvements is just not a great mediamagnet..
Another problem with not being there mentally, is that quality suffers. Our pilot in the video is probably not that hung up on doing "threepoint kissers" any more, "any landing you can walk away from son.." and so on..
Bottom line (finally) is: Imagine if we could motivate this old dog in the cockpit to get into the "training and structure" programme (the one that his less experienced colleagues rely on to get the job done.) How good and safe would not this guy fly planes?
Using really experienced anesthetists in CC-How good could it not be, getting these people off the "Gaze-heuristics", out of the "mental backseat", into the "training and structure" Wow..
You old-dogs, please,please,please: Start taking part in regular training and at least consider using a structured approach to critical procedures. With your experience sharpened by regular and structured training you can do both wonders and magic. Dont compare yourself to lesser experienced, compare yourselves to the highest imaginary standard You could possibly acchieve
And while we are at it - You Junior doctors (who still rely on a checklist to avoid crashing when you forget to lower the flaps - and you Will, sooner or later, with or without a checklist) PLEASE dont think that a checklist will keep you out of difiiculties or solve all of your problems, and PLEASE dont think that extensive training on a rubberduck is a substitute for clinical experience.
What the checklist and rubberduck training Will do is allow us all, old-dogs and novices alike, to deliver the best possible care at our level of experience, on every take-off.
That the world is changing goes without saying. Scandinavia has been hit as well.
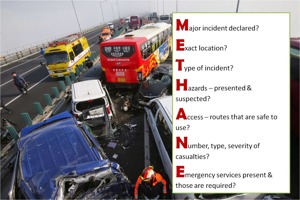
As critical care staff it is our duty to be prepared for anything. If we can not handle a serious event things will go south..
Being prepared for something that will hopefully not occur is challenging and requires commitment. We owe our community, countrymen and the world that commitment. For us in Sweden there is a real good opportunity to get a good introdution to the area of handling a serious and threatful event by some very experienced colleagues indeed. In october this event takes place.. See you there!
With increasing interest in tailored treatment för cardiac arrest patients There is a simultaneously increased interest in placing prehospital arterial lines.
This is encouraging and increases the potential for a higher quality of care for many types of patients in prehospital critical care. At the same time a lot of reactions questions the feasibility of the procedure. The placing of arterial cannulas is a clinical skill that needs to be perfected over years of experience, However, greater PHCC experience and the recent increased prehospital use of US makes placing arterial cannulas, even in moving vehicles and during CPR, quite feasible. The other hesitation concerns the setting up of arterial line sets. This is, no doubt, time consuming in a scenario that is already fitted in a tight timeframe.
Therefore it is with great pleasure we introduce a suggestion for a "Prehospital arterial line". A normal pressure dome where the "flushing set" is replaced with a normal 10 cc saline syringe. This cuts the preparation time for setting up the set to virtually zero. With the line in place flushing the syringe every 10 mins or so avoids any clot formation. An dditional advantage is that extra fluid lines and bags are minimized. The set is commercially available from several suppliers.
Invasive pressure is a Huge advantage in all critical patients, the prehospital world is no different.
Start monitoring your CC patients correctly and Know what you do.
Hospital quality PHCC! Your patients deserve it!
Tack för möjligheten att diskutera prehospital akutsjukvård och intensivvård med er! Jag hoppas att ni fortsätter den diskussionen på era hemsjukhus. Intemi nst kvaliteten på våra insatser på akutmottagningar och vårdavdelningar inom ramen för de "larm" vi springer på.. Kvaliteten på IVA ytansporter är ett annat ämne som vi inom speciliteten förr eller senare måste diskutera..
- Bifogat finner ni PDF på de flesta av mina föreläsningsbilder
- Bilderna från Mats föreläsning om Katatrofmedicin hittar ni här Lite extramtrl hittar ni här
- Socialstyrelsens Kamedorapporter med analyser av hanterandet av tidigare katastrofer/allvarliga händelser
- SMACC 2017 "das SMACC"
- Exempel på "FOAM" resurser med flera bra bloggar/podcasts
mvh
Joacim
In a recent editorial in Acta anaesthisologica Stephen Sollid et al comments on the recently published Scandinavian guidelines on prehospital airway management.
Focusing on competence more than formal specialty Sollid still notes that the anaesthesiologist has an especially good set of such competencies to acchieve safe and good prehospital airway management. However, he also states that both training and current hospital pracitice is necessary to reach the highest standards..
This of course applies to both hospital and prehospital "Critical Emergency Medicine". The challenge to Scandinavian anaesthesilogists has been stated by our emergency physician colleagues through Nicholas Aujalay in his blog post in sjukhusläkaren.
Now that challenge has been affirmed by a renowned and leading anaesthesiologist.
As anaesthesiologists providing critical care ("Critical Emergency Medicine") in hospitals we must respect the challenge of these clinical situations and stop sending our most junior colleagues to difficult situations without supervision and guidance!
As prehospial physicians we must uphold a current experience from hospital ICU/OR practice!
Finally regardless whether we practice in or outside of hospital we Must train for the job.
Anything less just wont do it anymore!
No effect..
We have all seen and read it: Yet another RCT that failed to show any significant outcome effect of MD delivered PHETI or perhaps yet another large study where ALS got beaten by BLS. We have all read them and probably also taken part in the frantic discussions of why that particular study failed. Frustratingly, the interventions studied are often accepted to improve outcome in hospital, such as TBI RSI or balanced fluid therapy or lately transfusions for bleeders.
In spite of same interventions..
Yet, it is really hard to understand why a resuscitative intervention that clearly benefits the patient when done in hospital would not be of benefit to the same patient earlier. Unless of course the intervention is done with reduced quality or done slower and hence with time lost. Could that perhaps be the case - we fail to prove effect of our interventions in prehospital critical care because we don’t deliver care of enough quality?
Hospital Quality as gold standard?
It is intuitively attractive to see critical care of hospital quality as the standard to strive for. After all, the hospital is where we deliver our critical patients.
How would this translate to real life? Wouldn’t it be satisfying to deliver our post-ROSC patients in a neuroprotective anesthesia, stable hemodynamics with beat to beat invasive monitoring of blood pressure, optimal ventilation on an ICU quality respirator with capnography. Diagnostics with 12 lead and UCG done, going for the cath lab or, rarely administering thrombolytics. The TBI patient safely anesthetized without hemodynamic instability, stable on a respirator, sedating drugs and possibly inotropes on the syringe drives. The MVC bleeder in deep, neuroprotective and dilating anesthesia getting blood products and procoagulative drugs while being delivered without delay to a level 1 trauma center. The septic meningitic patient sedated in a respirator getting EGDT and antibiotics/cortisone. The ICU transport getting the receiving hospitals level of care already during transport.
With the ability to deliver hospital quality prehospital critical care this is all quite possible.
Have we had the wrong focus?
Perhaps in the past we have been to eager to look at the effect of our interventions and in doing so forgotten about the quality of the interventions per se.
Instead of looking at the quality of our care per se we have been bogged down by meaningless arguments* of “what category of prehospital providers deliver the best prehospital critical care”.
If You do it, Make sure You do it well!
By accepting that the indications for prehospital critical care interventions are dependent not only on the pathology and the condition of the patient but also on our quality of care we can instead move forward together.
Let’s assume that the indication for a specific intervention is also proportional to the quality of the prehospital care compared to that of the hospital critical care. If we deliver critical care with the same quality as in the hospital where we will deliver the patient, clearly any early resuscitative measures we can take will benefit the patient (possibly even more than the, by necessity, later hospital intervention). Conversely, if we deliver care with reduced quality or with time lost we should probably be more cautious with the indications? At the extreme with only very low quality of care available, BLS is probably the best option?
With an accepted and common ambition of delivering hospital quality critical care, perhaps it is time to look at a process that has potential to lead to meaningful and beneficial such care? Importantly, this can of course be done regardless of the type of prehospital provider one uses.
What is HospQPHCC?
The first step in such an ambition would be to look at the components and abilities that make up hospital quality critical care. In itself, of course a very complex process. In its most simple form however this can probably be done in some sort of “activity” list. Defining the “toolbox” if you will.
Step 1-Activities in Hospital quality prehospital critical care
· Comparable medical competence
· System parameters, QA - M&M, CG etc
· Specific training
· Tailored treatment (as opposed to strict “protocols”)
· TBI Neuroprotective anesthesia (as opposed to protocolized drugs)
· Difficult airway capability – LMA, VL, surgical airway etc.
· Ability to perform advanced procedures – thoracostomies, -tomies and REBOA
· Capability to deliver “load&play” care enroute
· Syringe drives (as opposed to iterative boluses)
· Invasive blood pressure monitoring
· Capnography
· PRBC+FDP+TXA for bleeders
· Blood/Fluid warmers
· Topical hemostatics + Tourniquets
· “Hi-end” drugs, I.e. Inotropes, Thrombolytics, TXA, other procoagulative drugs, antibiotics, anesthetics, relaxants, analgesics etc.
· Diagnostics – Ultrasound, 12 lead ECG, ABG etc.
· etc.
The next step would be to look at the quality of care we deliver per se. One popular example is the first pass success rate with PHETI, but of course it is possible and probably necessary to identify several other quality indicators. For instance, even if a service delivers 100% first pass PHETI success rate, RSI desaturations and induction hypotensions as well as 30 min prolonged scene time may be harmfull to their TBI patients.
Continuing on the same metaphor quality indicators like this measure the ability to use the toolbox.
Step 2-Measurable quality indicators of hospital quality critical care
· First pass success rate with PHETI
· Correct indication for PHETI
· Desaturation with RSI
· Hemodynamic stability with TBI RSI
· Scene time for time critical conditions
· Correct PH triage
· etc.
The final step in this process would be to look at the effect of step one and two, i.e. mortality and morbidity studies. By not doing this until we have ascertained that we have the necessary “tools” for hospital quality PHCC (step 1) and the ability to use them properly (step 2) we maximize the likelihood of producing relevant studies
Step 3-RCTs comparing outcome of hospital quality critical care
· Mortality
· Morbidity
· Cost effectiveness
What we get out of it
Agreeing on accepted quality indicators would also enable us to better compare ourselves against each other and perhaps also define different levels of PHCC (in accordance with different levels of trauma and cardiology care) With a process like this and mutual inspiration it would allow different systems with varying prehospital providers to embark on a common journey that will produce better care and in the end the outcome studies we are all waiting for. Ultimately this will all benefit the patient.
Joacim Linde, MD, MSc




 0 kommentarer
0 kommentarer